Parathyroidectomy – Parathyroid Gland Removal Surgery
Minimally Invasive Parathyroidectomy (MIP) with Dr. Babak Larian
Dr. Babak Larian of the CENTER for Advanced Parathyroid Surgery specializes in minimally invasive parathyroidectomy (MIP) to treat hyperparathyroidism. MIP can be performed under local anesthetic in under 20 minutes via a small incision, and you can go home within an hour after the operation. As a parathyroid surgery expert, Dr. Larian always conducts an advanced 4 gland assessment to help his patients achieve the best results.
What Is a Minimally Invasive Parathyroidectomy?
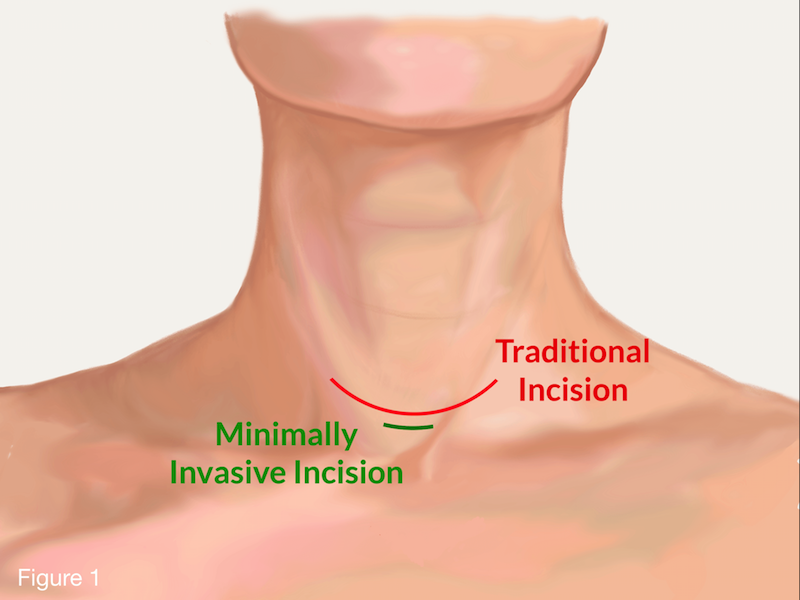
MIP has become the preferred method of operation for hyperparathyroidism, and it is an option for all patients considering standard parathyroid surgery. But what does MIP mean? Does it mean: A smaller incision? Less pain? Faster recovery? Local anesthesia instead of general anesthesia, without the need for a breathing tube? Less risk to vocal cord nerves? Less trauma to the tissue in the neck? Shorter surgery time? Not disturbing normal functioning parathyroids? Not staying at the hospital overnight? Potential of doing the surgery at an outpatient setting? Not at the hospital? Assessment of all four glands (Figure 1)? Higher cure rates? The answer to all these questions is YES.
Although it is often thought that minimally invasive surgery simply means a smaller incision, in terms of MIP, this is not the primary or sole objective. MIP‘s main objective is to cure hyperparathyroidism with as little disturbance of the tissue under the skin and other organs and structures (thyroid, vocal cord nerves, blood vessels, and normal parathyroids) as possible. Scar tissue will form in any area of the body that is operated on, and scarring can have long-term effects on the neck; as we speak and swallow, the voice box, trachea (breathing tube), and the area around the thyroid move up and down, and scarring can interfere with this important mechanism. Therefore, it is vital that the surgeon takes great care when operating on the parathyroid glands and does not interrupt or damage this delicate mechanism.
Additionally, the more extensive the surgery is, the greater the risk of damage to the recurrent laryngeal nerves (voice box nerve) and dormant shrunken parathyroid glands. A true MIP minimizes all of these risks, and it allows a patient to treat any form of primary hyperparathyroidism (single adenoma, double adenoma, or hyperplasia). It utilizes the latest techniques available to completely cure a patient (including intraoperative parathyroid hormone testing, pathology testing during surgery, and, when necessary, radio guidance, comprehensive neck exploration, or 4 gland exploration). The true advantage of Dr. Larian’s MIP with individualized 4 gland assessment is that each patient receives the care that is appropriate for him or her. No two patients are alike, and each deserves to be treated on a personalized basis.
Localization Studies
In order to do a true MIP, you must first find out which parathyroid has gone bad! Localization studies are done through studies such as an ultrasound, 4D parathyroid CT scan, sestamibi/SPECT scan, choline PET scan, or selective venous sampling to identify which gland is enlarged or producing excess amounts of calcium in the blood. Once the bad gland is discovered, surgery can then be focused on that gland without disturbing the remaining glands, the vocal cord nerve, and the thyroid on the opposite side.
4 Gland Assessment
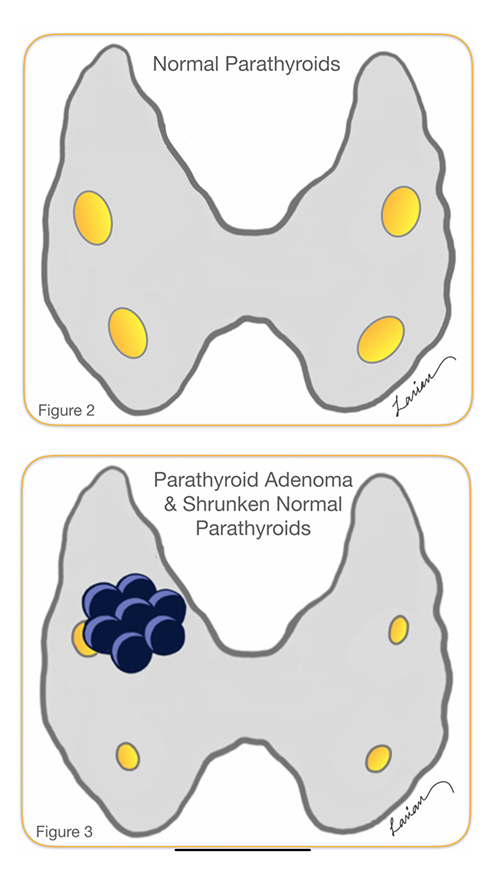
In the 1990’s, 4 gland assessment was done by looking at all four glands and doing a biopsy. However, this was fraught with problems because a biopsy did not always help doctors distinguish between a normal and abnormal gland. Additionally, when there is one parathyroid adenoma (a benign tumor in the parathyroid gland) that is overworking, the remaining three glands go into a dormant stage and shrink (Figures 2 & 3); this means looking for these smaller parathyroids and biopsying them can potentially be damaging and ultimately lead to permanent hypoparathyroidism.
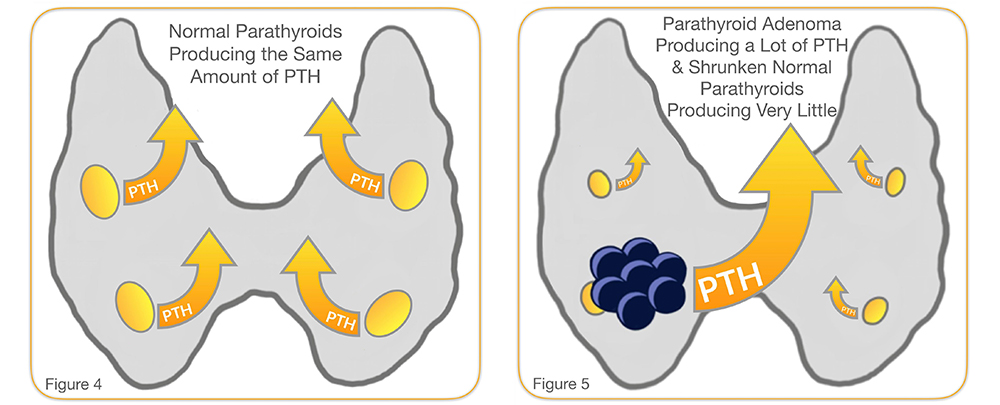
The modern version of a 4 gland assessment involves the removal of the enlarged gland and evaluation of the physiologic function of the remaining three glands by checking how much PTH that they are producing and putting into the bloodstream. The only accurate way to test PTH levels is by checking the amount in the bloodstream (Figures 4 & 5), and this is called rapid intraoperative PTH testing. After the removal of one gland, if the PTH level goes down by more than 50% in 10 minutes, then the remaining glands are dormant. If the PTH level does NOT go down by 50%, then that means one or more of the remaining glands is abnormal and should be investigated. This is very important because it is estimated that up to 25% of people with hyperparathyroidism have more than one gland that is abnormal. Without PTH testing, 75% or more of the people who have only one abnormal gland would have extensive bilateral surgery unnecessarily.
Parathyroidectomy Surgical Steps
- PTH level testing is performed in a pre-surgery unit while placing the IV
- Patient comes into the operating room and lays flat on the bed
- Intravenous sedative (through the IV), and the patient falls asleep while breathing on his or her own (NO BREATHING TUBE NEEDED). This is an option, as patients rarely choose to be fully awake
- Local anesthetic is given to the patient
- The patient’s skin is cleaned and sterilized
- Surgery
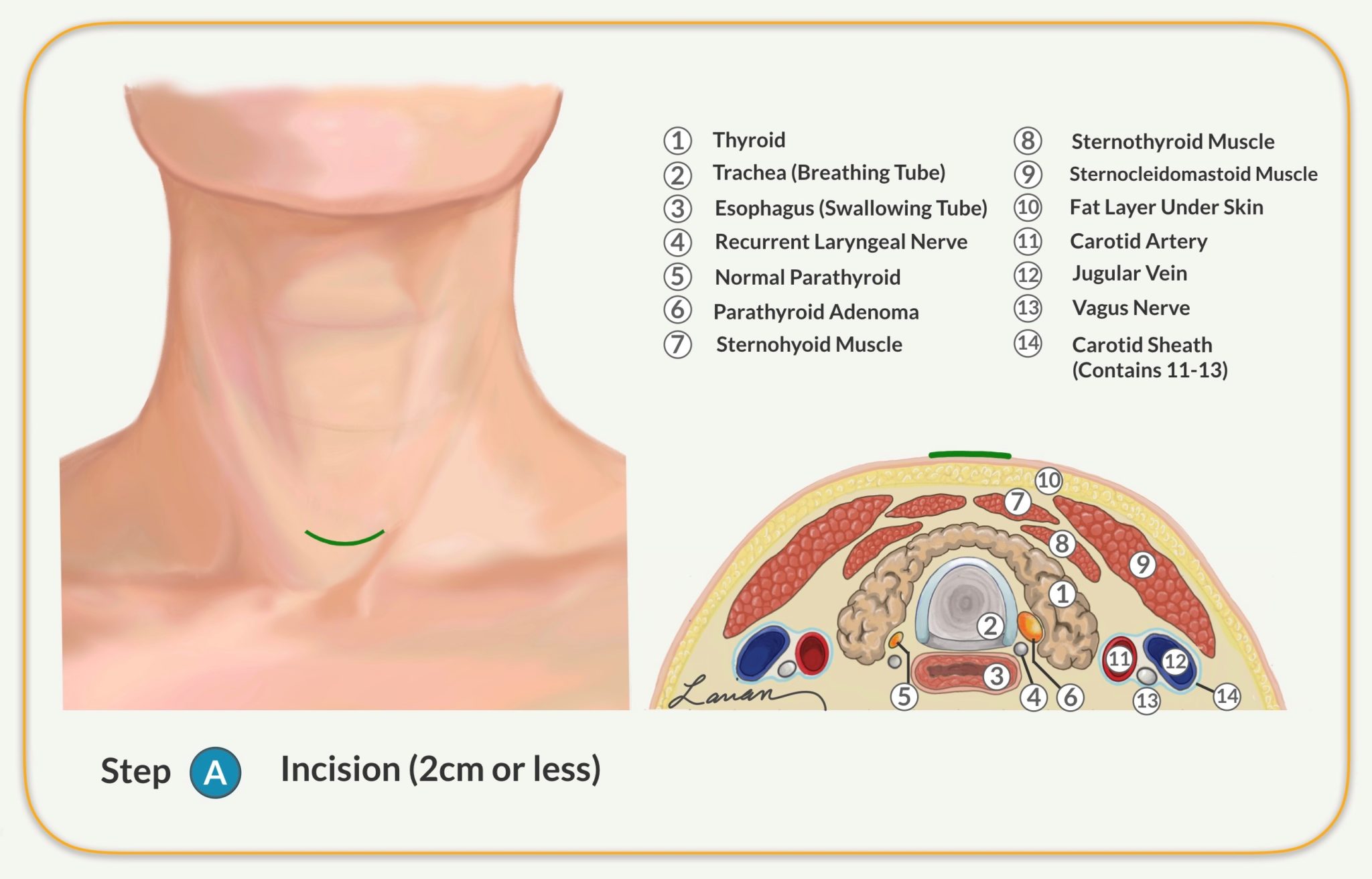
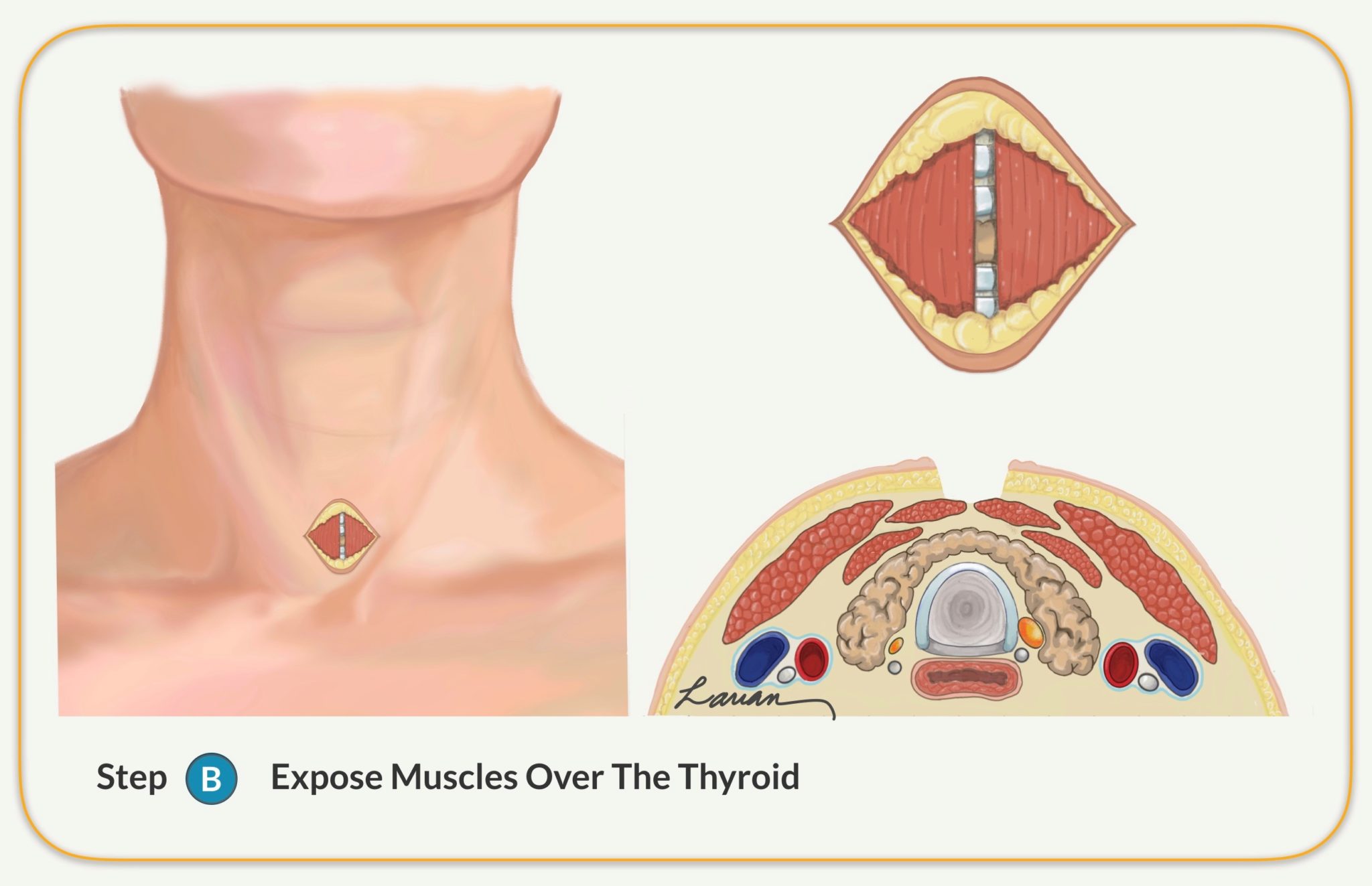
- Involves an incision of 1.5 to 2 cm (less than an inch)
- Exposes the sternohyoid muscle (covering the thyroid and trachea)
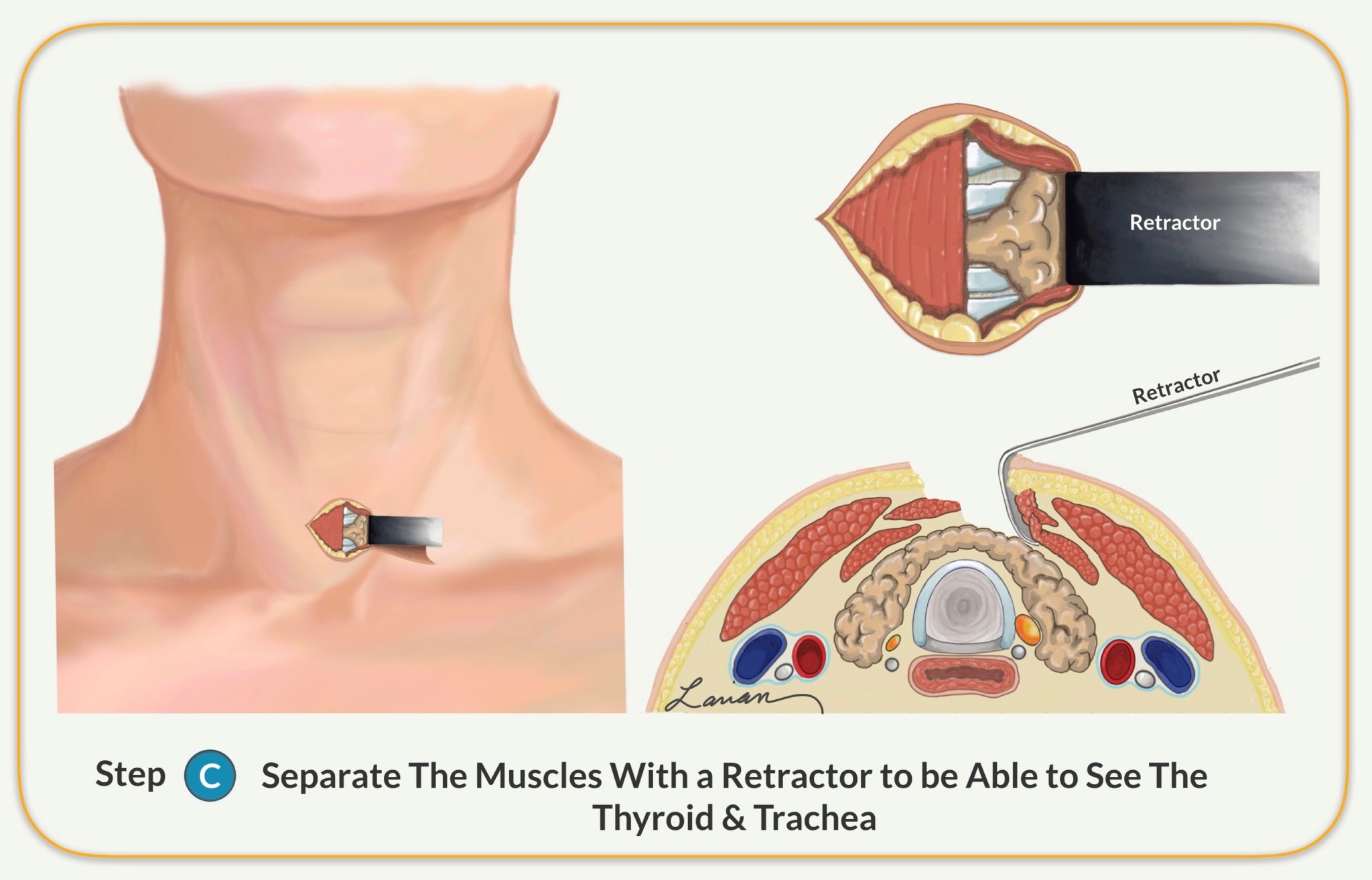
- Separates the thin muscles from over the thyroid (not cutting the muscle) on the side where scans showed the abnormal parathyroid gland is located
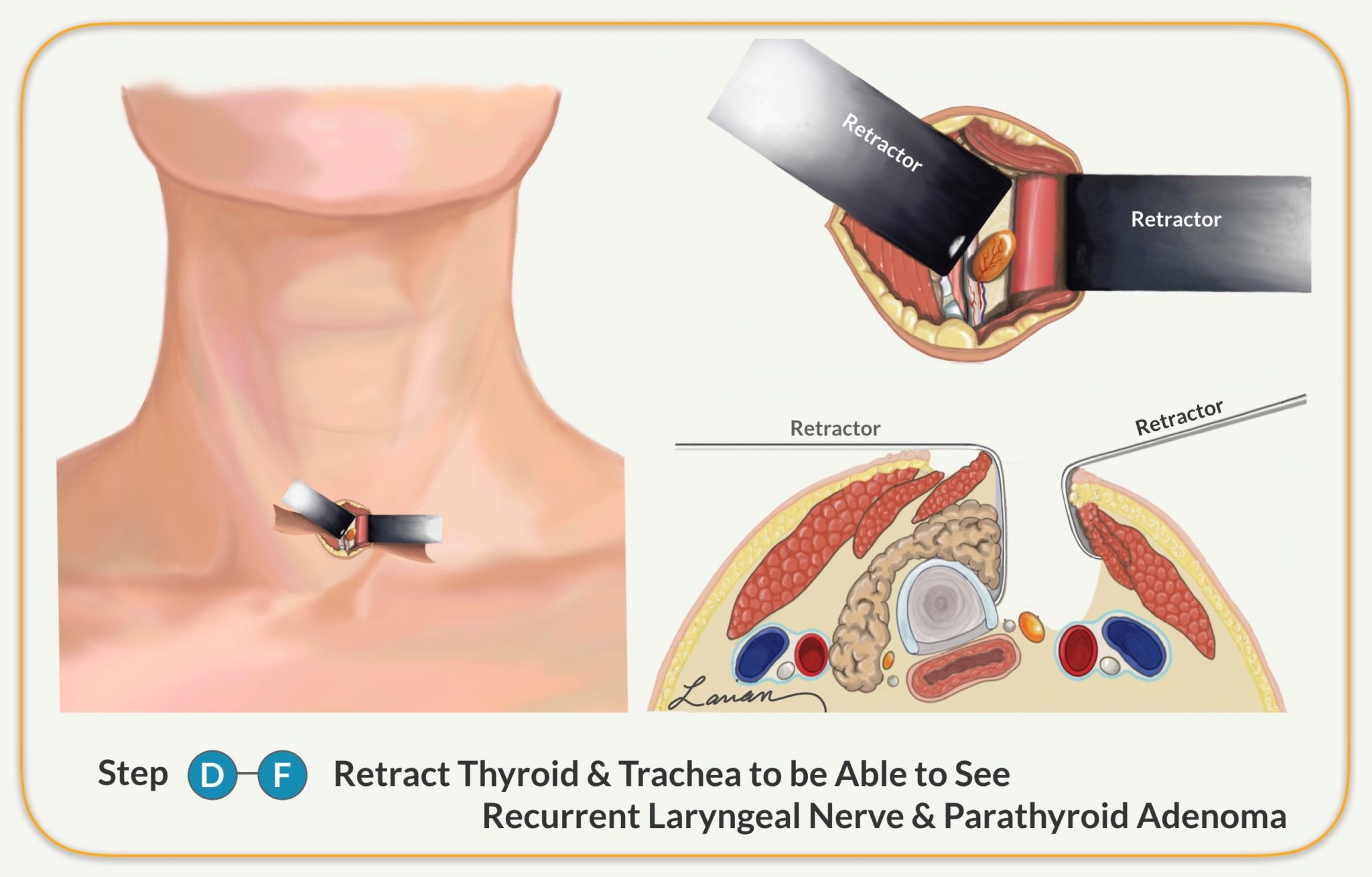
- Allows the surgeon to find the recurrent laryngeal nerve (RLN) deep to the thyroid
- The surgeon follows the RLN and protects the nerve
- The surgeon dissects the abnormal parathyroid gland and separates it from the thyroid, lymph nodes, and fatty tissue
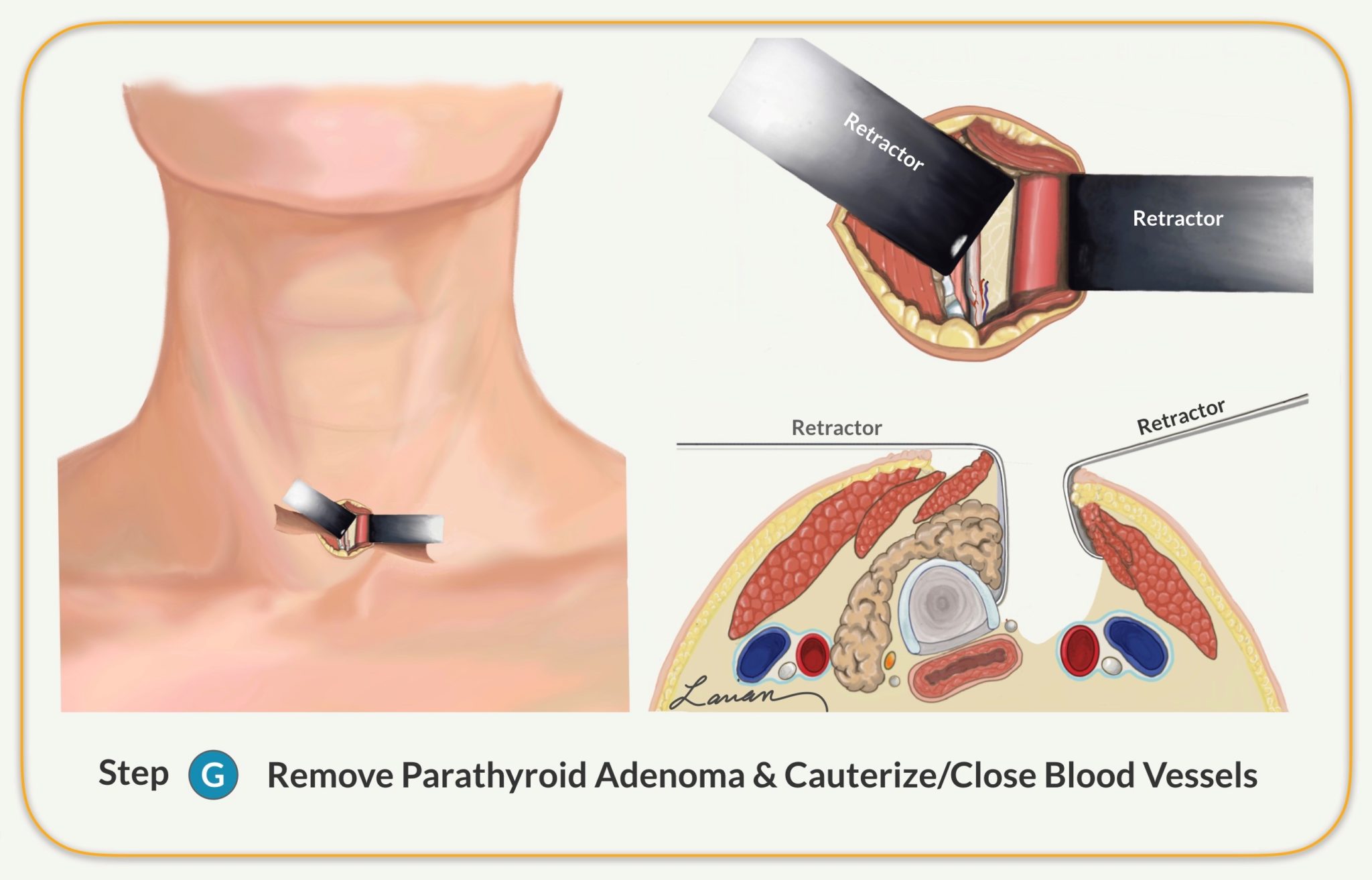
- The surgeon identifies the blood vessel that feeds the abnormal parathyroid and clamps and closes the vessel
- The surgeon checks the patient’s PTH level at 10 and 15 minutes to make sure it goes down by more then 50% and stays low
- The surgeon examines the area to make sure there is no bleeding from the small blood vessels
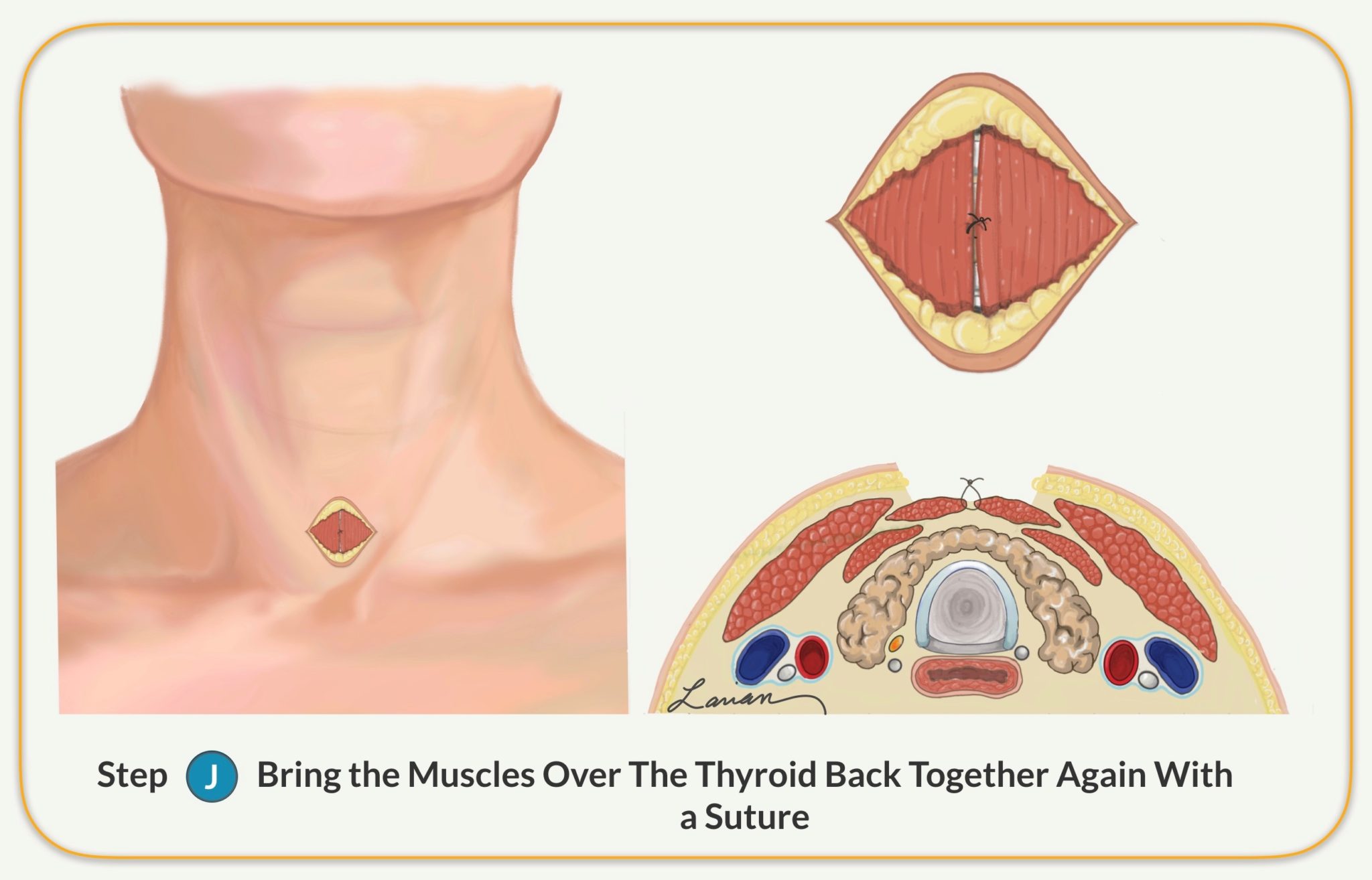
- The surgeon brings the muscles over the thyroid together again
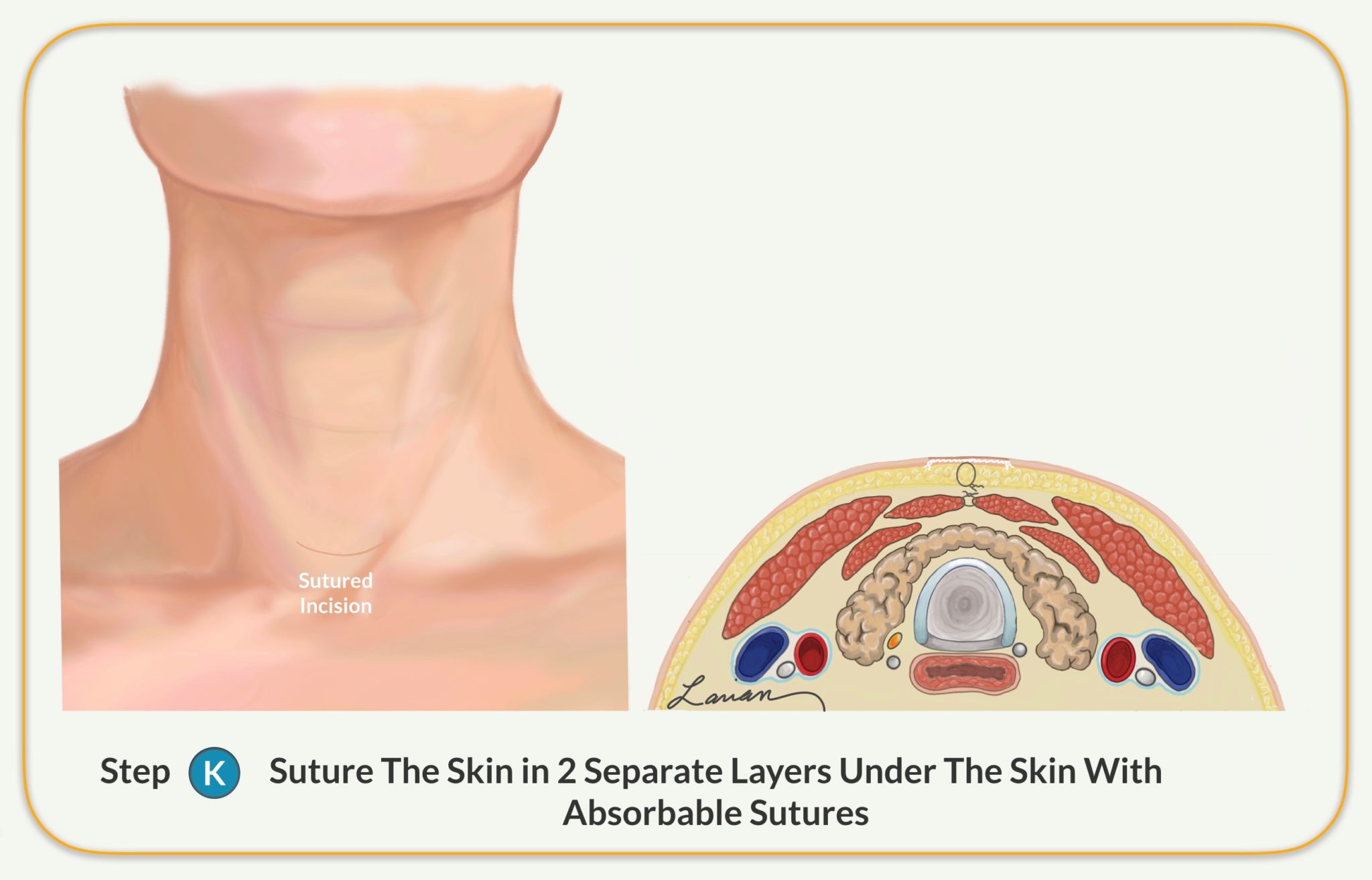
- The surgeon sutures the skin close in multiple layers with absorb-able sutures that are under the surface
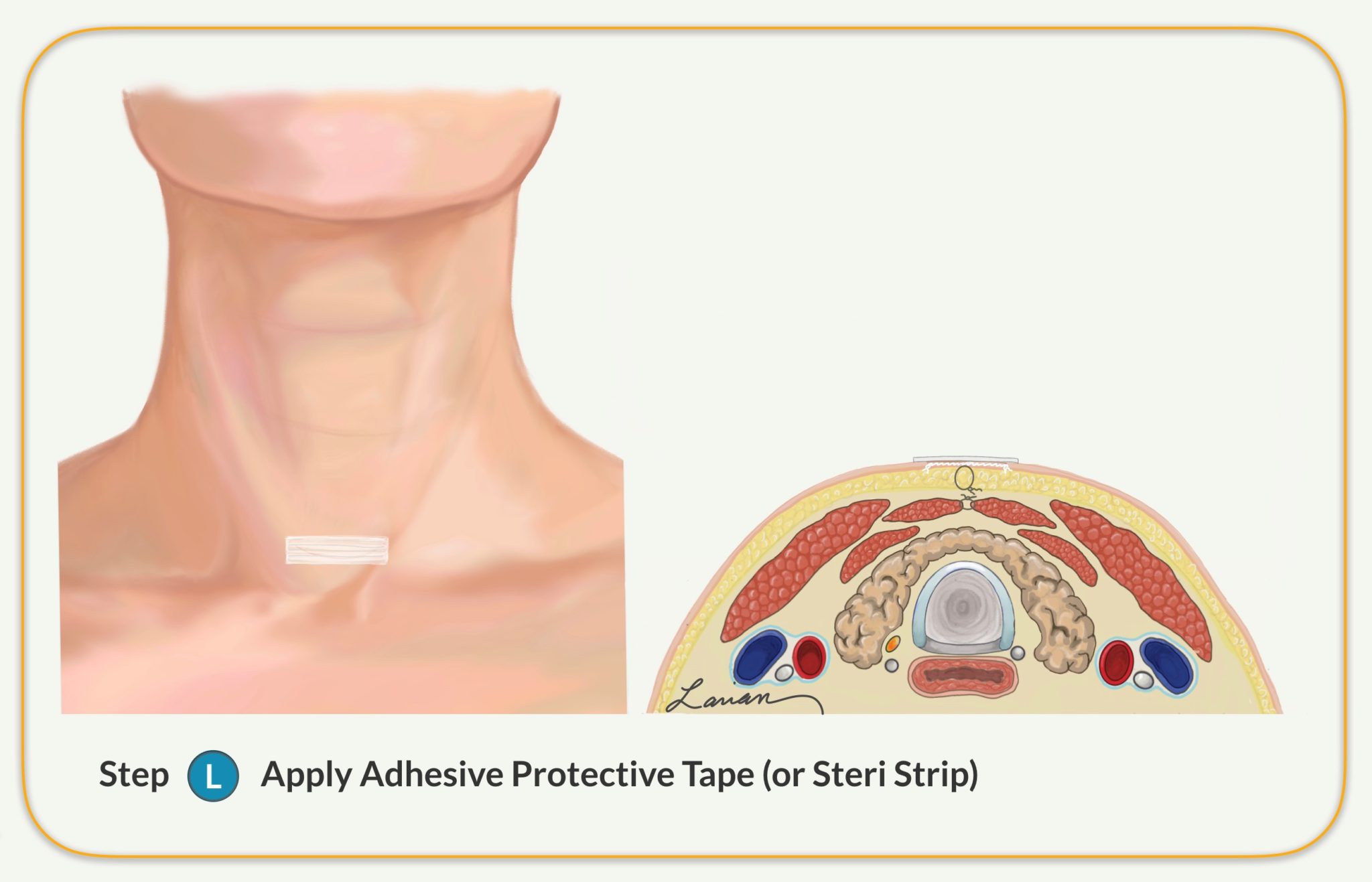
- The surgeon places a steri-strip (medical grade tape) on the incision for added protection
- The surgeon wakes up the patient and takes him or her to the recovery room
- The patient remains in the recovery room until he or she is fully awake
- The patient is released to go home usually after an hour
Average Operative Time is Less Than 20 Minutes
MIP involves minimal anesthesia and helps patients avoid unnecessary scarring, and it is a fast procedure. Using this technique, the average operative time is less than 20 minutes; by comparison, a standard parathyroid surgery that takes two hours or more to complete. With MIP, almost all patients are sent home within an hour or two of the operation. Most importantly, the complication rate of MIP is less than half compared to the standard option.
Parathyroid Gland Surgery Risks
Risks associated with parathyroid surgery include:
- Laryngeal nerve injury: Injury to the nerve that controls the vocal cords is very rare; it may result in a hoarse voice.
- Low blood calcium: Damage to the parathyroid glands sometimes results in low calcium levels following surgery; in this instance, calcium and vitamin D supplementation may be required to help a patient replenish his or her calcium level. This is most often temporary and will resolve after a short time with calcium & vitamin D replacement. However, in some cases this can be a permanent consequence of surgery.
- Bleeding: Just as in all surgeries there is a risk of bleeding, but due to the fact that the parathyroid vessels are smaller caliber the risk is small (less than 1%). This is a medical emergency and the person needs to immediately call the paramedics if it were to occur.
- Infection: Just like any surgery there is a possibility of infection, however due to the fact that the neck has an abundant blood supply that bring a lot of nutrition and immune fighting cells, the chance of infection is low. So much so that antibiotics are only needed for patients that have complex medical problems or implants.
Choosing an experienced, board-certified surgeon with extensive experience operating in the neck to perform parathyroidectomy is key. This surgeon devotes the time and resources to minimize risk and ensure a patient can achieve the best-possible treatment results.
General Instructions for Your Parathyroidectomy Pre-Admission Testing
All patients scheduled for surgery must have the following tests done at the facility of their choice up to one month before their planned surgery:
- Chem 7, CBC, PT, PTT (within one month of surgery)
- EKG & Chest x-ray (age 50 and above, accepted up to 6 months prior to surgery)
The Day of Surgery
Timing Your Arrival
Please plan to arrive at La Peer Surgery Center 1 hour prior to your surgery time, or Cedars-Sinai Medical Center at least two hours prior to your surgery time. You will be called by the hospital or surgery center to confirm your surgery on the day prior to your surgery. If the hospital or surgery center has not called by 4:30 pm that day, please call our office.
Food & Drink
Do not eat after midnight before your planned surgery. You can have clear liquids up to eight hours before surgery. You may take your usual asthma, heart, blood pressure, or seizure medication with a small sip of water that morning unless otherwise advised.
Medications
Please do not take any aspirin, ibuprofen, Alleve, or other over-the- counter pain medications for one week before your surgery. You may use Tylenol in the week before surgery. If you are a diabetic, consult
with your physician before taking your medication. Also, if you develop a cold, sore throat, fever or any illness, please call Dr. Larian’s office prior to your surgery.
Parathyroidectomy Recovery
There are many things that patients can do to ensure seamless recovery after parathyroidectomy surgery, including:
- Prioritize Self-Care: Patients should not overexert themselves in the first few weeks after surgery. They should try to walk daily to improve blood flow but should not engage in strenuous activity or lift heavy objects for at least three weeks after surgery.
- Consume Healthy Foods: In the first 24 hours, it’s best to eat simple bland foods that wont upset your stomach and cause nausea. In some instances, patients experience pain with swallowing immediately after surgery. These patients should consume soft foods like pudding and yogurt and avoid hard and scratchy foods like chips and raw vegetables until swallowing becomes more comfortable. Your body needs protein & vital vitamins and minerals to heal the area of the surgery, so please make sure you are getting a good supply of protein, as well as fruits and vegetables.
- Control Pain: The pain after Parathyroidectomy is usually minimal, such that close to half the patients either only take Tylenol or no medicines at all. However, Dr. Larian recommends that whatever your pain level is to appropriately manage it, and take medications as needed & instructed to control pain. Control of pain is an important part of healing.
If there are concerns or questions during parathyroidectomy recovery, it is essential to reach out to Dr. Larian for assistance. Dr. Larian strives to do everything to help his patients, and he is happy to respond to any concerns or questions at any point during the surgery recovery process.
Parathyroidectomy FAQ
If you need parathyroid surgery, it is important to know what to expect. The following are some of the most frequently asked questions about parathyroidectomy:
- How will I know if I’m a good candidate for parathyroid gland surgery? MIP is ideal for nearly all parathyroid tumors. To determine if a patient is a good candidate for MIP, Dr. Larian meets with him or her and performs an evaluation. If Dr. Larian believes MIP is the best option based on a patient’s symptoms, he then recommends MIP.
- Are numbness and tingling common side effects associated with parathyroid surgery? Some patients experience numbness and tingling in the lips and fingers following surgery. These symptoms may occur due to a reduced level of calcium in the blood. Once a patient’s calcium level returns to a normal level, numbness and tingling should stop. If these symptoms persist, it is important to contact Dr. Larian for additional support.
- Will MIP help reduce fatigue? Research indicates parathyroid surgery has helped many patients reduce fatigue and enjoy a better quality of life.
- Can MIP help improve memory? Research indicates some hyperparathyroidism patients deal with impaired memory. Meanwhile, research shows that hyperthyroidism patients sometimes experience improved functioning across memory, attention, and reasoning after surgery.
- Is MIP an effective treatment for kidney stones? MIP cannot be used to repair existing kidney stones. On the other hand, MIP may help reduce the risk of future kidney stones in patients dealing with primary hyperparathyroidism and kidney stones.
- Does MIP help patients improve their bone density? Research indicates parathyroid gland surgery sometimes helps patients improve their bone density by as much as 12%. Parathyroid surgery has also been shown to help reduce the risk of bone fractures.
- What type of anesthesia will I have? Most people are able to have local anesthesia with or without a small amount of sedation (relaxation medicine) for parathyroid surgery.
- How long will I be hospitalized? Parathyroidectomy does not require hospitalization unless there are other medical issues such as heart, lung or kidney disease. Most patients go home after spending between one to three hours in the recovery room and feel well enough to travel to their home or hotel.
- Will I have pain after the operation? Some pain is common because we are not cutting muscles or major organs. Most patients are able to manage the pain with Tylenol.
- What are the advantages of minimally invasive parathyroid surgery? The advantages of minimally invasive parathyroid surgery over the standard option include less trauma to the tissue under the surface, as well as less trauma to the thyroid, remaining normal parathyroid glands, and less chance of injury to the vocal cord nerves.
- How big is my incision? The incision ranges from 1.5 to 2 cm (less than an inch).
- Will I have a scar? That depends on your healing properties, but the chances are exceeding low that you will have a visible scar.
- What is the purpose of the pre-surgery tests? These tests are used to identify the abnormal (or bad) parathyroid gland.
- Will I have stitches? Yes, but all of the stitches will be located under the skin. They also dissolve on their own and don’t need to be removed.
- When will I know the findings of the surgery? Immediately after surgery, you will have preliminary results, and three working days later, you will receive the final pathology report.
- Will I have any physical restrictions after surgery? Yes, we suggest no strenuous exercise for two to three weeks after surgery so as to not cause a quick rise in your blood pressure or a healing blood vessel to open and bleed. However, we do not want you to be in bed during the day, but instead, you should remain slightly active and go for walks twice daily to get the blood circulating so as to help rebalance the body sooner.
- What are the complications and possibilities unique to parathyroid surgery? The most common ones (although still rare) are: Not finding the abnormal (bad gland), which can occur if the gland is in an unusual place (in the chest for example) that was not visible on the scans before surgery, and vocal cord nerve injury, which happens in less than 1% of cases.
- What is the recovery time for parathyroid surgery? Usually within the first 24 hours after surgery, patients can be active once again, but we suggest not returning to work for five days following treatment. The length of time to fully get back to balance has to do, most likely, with how long you have been dealing with hyperparathyroidism and your calcium level.
- Can hyperparathyroidism cause you to gain weight? It can, mostly because of its impact on energy levels, muscle strength, and motivation to do anything.
- What happens if parathyroid disease goes untreated? Lots of possible complications, including loss of bone (osteoporosis), bone fractures, progressive mental slowing, fatigue, kidney disease, an increased chance of certain cancers, etc.
- What foods should I avoid if I have hyperparathyroidism? None.
- Does vitamin D3 replacement before surgery help? Yes, if tolerated (a certain percentage feel worse), it can help decrease hungry bone syndrome and make post-surgery calcium management a bit easier.
- Are there any dietary restrictions during parathyroidectomy recovery? Most patients can resume a normal, balanced diet after surgery. Patients should also drink plenty of fluids following surgery.
- What happens to parathyroid tissue that is removed during surgery? Parathyroid tissue is evaluated after surgery; this allows Dr. Larian to identify any abnormalities, including cancer. Dr. Larian then meets with a patient to share the evaluation results.
- What happens if cancer is discovered in parathyroid tissue after surgery? The chance of incidentally finding parathyroid cancer is very low because parathyroid cancers tend to produce a lot PTH and can be detected on lab testing before surgery. Early detection is paramount when it comes to treating parathyroid cancer. Chemotherapy and radiation therapy often fail to help parathyroid cancer patients, and these patients may require repeat operations if the disease continues to come back. Conversely, if parathyroid cancer is discovered in its early stages, it may be possible to remove the cancer successfully.
- Do I need to make a postoperative appointment after surgery? For patients who live locally, Dr. Larian encourages them to follow up at least once after surgery. For those coming from out of town or country, this can be done via phone or video conferencing.
For More Answers, Watch Dr. Larian’s Hyperparathyroidism FAQ on Facebook Live
Schedule a Consultation with Dr. Larian Today!
To learn more about parathyroid surgery or schedule a treatment consultation with Dr. Larian, please call us today at 310-461-0300.









