Abnormal calcium levels in the bloodstream characterize hyperparathyroidism. Each person needs a unique calcium level to function at peak capacity. When that level fluctuates, it can lead to uncomfortable symptoms and potentially serious complications. This condition can be categorized as primary or secondary hyperparathyroidism.
What Is Secondary Hyperparathyroidism Disease?
While primary hyperparathyroidism (PHPT) begins with an enlargement of one or more parathyroid glands, secondary hyperparathyroidism is caused by another medical problem, like a vitamin deficiency or kidney failure. This underlying condition leads to lower blood calcium levels, which impact the parathyroid glands’ function. The glands do not usually enlarge with secondary hyperparathyroidism unless the disease progresses.
Because PHPT originates in the parathyroid glands, they are targeted for treatment. Surgery to remove all or a portion of the glands is typically the best method of reversing primary hyperparathyroidism. However, secondary hyperparathyroidism treatment needs to focus on the underlying problem first to restore calcium levels and parathyroid function. In advanced cases, surgery may also be recommended to remove parathyroid tissue.
Causes of Secondary Hyperparathyroidism
Underlying medical issues that can lead to hyperparathyroidism include:
Calcium Deficiency
Calcium is an essential mineral that keeps teeth and bones strong, promotes healthy blood flow, and assists with nerve messaging between the brain and body. A calcium deficiency may occur when your digestive system no longer absorbs calcium from your food as efficiently. This can sometimes happen after intestinal or bariatric (weight loss) surgery. Calcium deficiency might also result from chronic diarrhea due to conditions like Crohn’s or celiac disease.
Vitamin D Deficiency
Vitamin D is a critical nutrient that maintains healthy calcium levels in the blood and helps the intestines absorb calcium from food. A large portion of the population is vitamin D deficient, and needs to supplement. Common causes of a vitamin D deficiency include:
- Lack of vitamin D-rich foods in the diet
- Limited sun exposure
- Inability of the liver or kidneys to convert vitamin D
- Medications that disrupt the absorption of vitamin D
Kidney Failure
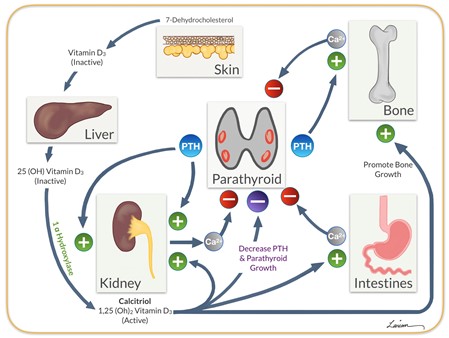
Kidney failure is the most common cause of secondary hyperparathyroidism. Healthy kidneys convert vitamin D so they can absorb calcium from food. When kidneys become diseased, they can no longer activate vitamin D, leading to a decline in blood calcium levels. The parathyroid glands try to adjust calcium levels by producing more parathyroid hormone (PTH). PTH tells the bones to release calcium, and the kidneys to take calcium out of the urine and put it back into the bloodstream.
While this process can raise calcium levels, it also strains the parathyroid glands as they work overtime to release more PTH. Over time, the parathyroid glands can enlarge and produce too much PTH, raising calcium to a dangerous amount in the bloodstream. At this point, surgery is often necessary to remove all or part of the gland to restore normal PTH and calcium levels.
Symptoms of Secondary Hyperparathyroidism
Secondary hyperparathyroidism symptoms mimic those of PHPT and might include:
- Ongoing fatigue
- Joint and muscle pain
- Difficulty concentrating
- Memory problems
- Depression and anxiety
- Stomach pain and nausea
- Increased thirst
- Frequent urination
It can be challenging to diagnose hyperparathyroidism based on symptoms alone since these signs are nonspecific and may be attributed to numerous medical conditions. A parathyroid expert will know which tests to use to diagnose the condition and determine the correct treatment.
Diagnosing Secondary Hyperparathyroidism
Diagnosing either type of hyperparathyroidism can be challenging since PTH and calcium levels can vary significantly from patient to patient. A secondary hyperparathyroidism diagnosis usually involves tests to assess blood calcium, PTH & vitamin D levels, creatinine levels in the blood, calcium levels in the urine, and bone mineral density. In addition to diagnosing hyperparathyroidism, the underlying cause needs to be identified since this will determine the right treatment path.
Current Treatments for Secondary Hyperparathyroidism
The best secondary hyperparathyroidism treatment depends on the underlying cause of the disease. When kidney disease is the culprit, it is known as renal hyperparathyroidism and is typically treated with vitamin D supplementation and dialysis. A parathyroid expert and a nephrologist often work together to ensure the patient receives comprehensive care.
If calcium malabsorption has caused the problem, calcium and vitamin D supplementation is usually prescribed until PTH levels return to normal. A parathyroid expert should oversee this treatment since it can take time for levels to stabilize. If the parathyroid glands have enlarged, surgery may also be recommended to remove the affected gland.
Managing Complications and Outcomes: When To See A Specialist
Secondary hyperparathyroidism can be challenging to diagnose, but if left unchecked, it can become dangerous and even deadly. Working with a parathyroid specialist who knows how to diagnose and treat this condition correctly is critical. Dr. Larian has helped hundreds of patients find relief from hyperparathyroidism symptoms and improve their quality of life through effective treatment options. Contact us today to learn more or schedule your consultation with a member of our team.









